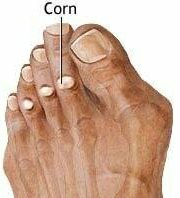
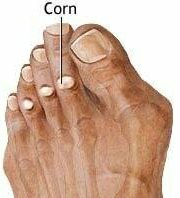
What is a corn?
|
|
Corns are areas of hard, dead skin that form in response to abnormal shoe pressure and friction. Corns can become inflamed and painful if the shoe pressure continues. But a corn is just a symptom of some underlying toe pathology, such as: |
|
Hammertoes: Toes, which are bent so that the part closest to the foot is directed upwards, while the remainder of the toe is bent down, so that you walk on the tip of the toe. Corns may form on the top of the toe where the shoe rubs against it. Or they can form on the tip of the toe, because you do not apply weight to the entire toe when walking, but just to the tip. Click here to learn more about hammertoes.
Bone Spurs: A benign bone mass (extra bone) usually occurring between the toes. The bone spur places increased pressure on the overlying skin of the toe and the adjacent toe. The resulting pressure causes a build-up of hard, dead skin (a corn), which becomes painful when shoes are worn as the toes rub against one another.
Of Note: Corns not treated in patients who may be neuropathic and or diabetic may not feel the discomfort of the corn. These patients are at risk for ulceration of the affected corn. Ulceration may be serious as it can cause infection to reach the underlying bone. Ulceration in vascular compromised patients can lead to serious complications including infection and even possible amputation.
Hard corns (heloma durums) are the most common type. They are caused primarily by ill-fitting shoes and toe deformities such as hammertoes. They usually develop on the tops and tips of toes. These corns are usually hard and dry.
Soft corns (heloma molles) usually are the result of bone spur formation in the toes. They are found between the toes and usually are white in color and frequently appear moist or macerated.
What Are The Differences Between Corns and Calluses? The two biggest differences are the location and size of the lesion. Corns are small and round and are located on the top, tips, or between the toes. Calluses on the other hand, are larger, flatter, and can be found on the bottom of the feet.
-
Symptoms
-
The symptoms produced by a corn vary according to:
How thick and hard the corn is.
The amount of shoe friction or pressure it is subjected to.
The thicker the hard dead skin of the corn, and the more it is irritated, the more noticeable are the symptoms.
Common symptoms of corns include:
Pain in the corn and surrounding toe joint.
Inflammation of the irritated skin and/or corn.
Thick, hard, rough, dry skin on the tops or tips of the toes. Tenderness or pain under the skin and corn.
Soft corns form between the toes and usually appear white or flesh colored.
Corns may have a hard, dry plug, or nucleus in their center. These plugs can extend deep into the top layers of skin, often pressing on superficial nerves and causing increased pain. Because of the shape of these plugs (funnel shaped – broad raised top and a pointed tip at the bottom), corns intensify the pressure at the tip and can cause deep tissue damage and ulceration. Hard corns are especially problematic for people with insensitive skin due to diabetes and peripheral neuropathy.
-
Causes
-
Corns are caused by excessive pressure or friction on the toes, usually from ill-fitting shoes or high heels. Since the skin acts as the body’s protector, corns form when the body attempts to protect the irritated area from more pressure by building up a mass of dead skin cells and secreting a hard substance called keratin. When this mass of dead cells is thin there is usually no pain. However, as the shoe pressure and friction continues to irritate the toe, the dead cells become thicker and harder, and eventually they may become painful and inflamed.
Predisposing Factors: Those factors, which increase your chances of developing corns:
Hammertoes
Bone spurs
Arthritis
Rigid feet with high arches
Presence of other foot deformities such as bunions
Toe injuries, fractures, and dislocations that were not treated properly
-
Treatments, Self-Help, & Prevention
-
Daily inspection of the feet in patients whose feet are insensitive due to Diabetes or neuropathy should be conducted.Inspection of the feet should also be included in those patients who have some evidence of circulatory disorders.
Regardless of the cause, the painful corn must be protected from shoe pressure for the pain to subside. Buying shoes with a wide and deep toe box (the part of the shoe where the toes sit) may give some relief. The following remedies are prescribed by doctors to relieve shoe pressure, toe pressure, and pain in these toes, or to help the toe lie straight, thus alleviating pain and preventing the corn from becoming worse:
Relief and prevention of corns due to hammertoes (corns that form on the top and tips of toes):
Kerasal One Step Exfoliating Moisturizer Therapy gently exfoliates and softens hard, dry, dead skin.
Budin Hammertoe Splints extend the hammertoe and allow it to lie straight; thus, pain is alleviated in the top and tip of the toe.
Removable, long lasting Crest Pads straighten the toes and prevent them from rubbing against the tops of your shoes, relieving your pain.
Removable, comfortable, and long lasting Gel Toe Pads
Artemis Woman Heel Smoother (Approved by the APMA) pedicure appliance smoothes calluses and removes dry skin on heels and toes in seconds, without the use of harsh chemicals or dangerous blades.
Exercise by stretching the toe straight for 10 seconds, and repeat for 3 to 5 minutes daily. Wear longer shoes. Wear flat shoes. (Do not wear shoes with a heel higher than 3/4 inch).
Gentle massage with a cool liniment will help to relieve your pain.
If you ever experience open wounds, intense redness, or extreme pain, see a podiatrist immediately.
Relief and prevention of corns due to bone spurs (soft corns that form between toes):
Adhesive foam corn pads. Use to protect painful and irritated areas on toes. Made with medical grade foam.
Removable, long lasting Digital Toe Caps. Slips over entire toe to ease discomfort from hammertoes and ingrown toenails. Cushions sore deformed toes and relieves pain.
Gel toe separators and spreaders comfortably prevent toes from rubbing against each other, thus eliminating friction and pain.
Foam toe sleeves will shield your toes from pressure and friction.
Wear shoes with a wider toe-box.
Wear flat shoes.
Do not wear socks or stockings that are tight.
If you ever experience open sores, extreme redness, or extreme pain, see a podiatrist immediately.
Self-treatment with the use of razor blades, knife blades, or nonprescription preparations of acids should not be attempted because of the risk of injury and infection.
If Conservative Care Fails
If conservative treatments fail and your symptoms persist, the doctor may recommend a surgical option. The procedures vary greatly, depending upon the reasons for the corn. If a hammertoe is responsible, the podiatrist can perform surgery to straighten the toe. There are a number of different operations to straighten the toe, the most common ones involve:
Soft tissue corrections such as tendon transfers, tendon lengthening, and joint capsule repairs.
Digital arthroplasty involves removal of bone from the bent joint to allow the toe to straighten. The temporary use of pins or K-wires may be necessary to keep the toe straight during the healing period. Joint implants are sometimes used to allow for a better range of motion in the toe following surgery.
Digital arthrodesis involves the removal of bone from the bent joint and fusing the toe in a straight position. If the corn is due to a bone spur, the most common procedure used is an exostectomy, in which surgically removing it or filing it down removes the bone spur.
Because of the possible complications involved with any surgery, one should be sure to understand the risks that may be involved with surgery to treat corns, correct hammertoes, and remove bone spurs.